Candida auris, also called Candidozyma auris, is an emerging yeast that has raised alarms in hospitals. Discovered in Japan in 2009, it has since spread worldwide. What makes Candida auris special: it is often multidrug-resistant—insensitive to common antifungal medications. The fungus can cause life-threatening infections in immunocompromised patients and has prompted increased vigilance by public health authorities. The U.S. CDC classifies Candida auris as an “urgent threat” to public health. Below we explain what Candida auris is, how it spreads, who is at particular risk, and how infections can be prevented [3].
What Is Candida auris?
Candida auris is a species of yeast (Candida) that can cause human infections. It was first described in 2009 when it was detected in the ear (auris) of a patient in Japan. Unlike many other Candida species (e.g., Candida albicans), Candida auris is not a harmless part of the normal skin or gut flora.

New designation: Based on newer taxonomy, Candida auris is now assigned to the genus Candidozyma. You will therefore often see Candidozyma auris (formerly Candida auris).
Key Characteristics
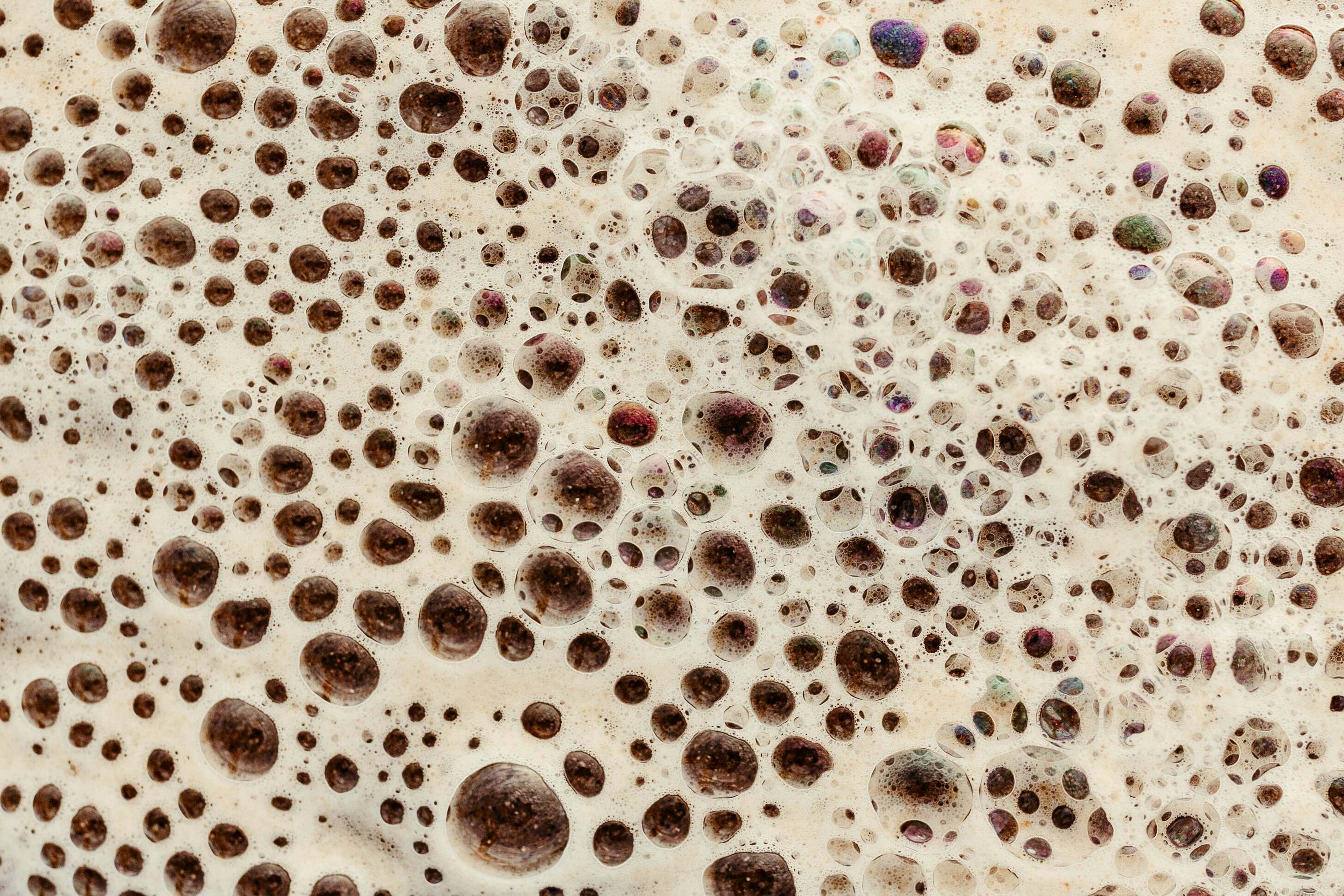
It grows on specific culture media as a gray-white, persistent coating and can be easily mistaken for other yeasts. Modern diagnostics are required to identify C. auris reliably [1,3,7].
Why Is Candida auris So Dangerous?
Candida auris is concerning for two main reasons: high transmissibility and multiple drug resistance.
- Highly transmissible: The fungus can be transmitted from person to person, especially in hospitals and long-term care facilities, and can persist on dry surfaces for weeks.
- Multidrug resistance: Over 90% of investigated strains are resistant to fluconazole, ~30% to amphotericin B, and some also to echinocandins. In rare cases, strains are resistant to all available agents.
Infections are often recognized late because symptoms are nonspecific. Case-fatality rates can reach 30–60%. In 2022, WHO placed Candida auris in its highest priority tier (critical).
Comparison with Common Candida Species
| Aspect | Candida albicans | Candida auris |
|---|---|---|
| Natural occurrence | Part of normal body flora | Not part of normal flora; healthcare-associated |
| Transmission | Endogenous infection | Nosocomial contact transmission; not airborne |
| Resistance | Usually susceptible to standard antifungals | Often multidrug-resistant; sometimes no effective drugs available |
| Typical diseases | Superficial infections (e.g., oral thrush) | Invasive infections with high mortality (up to 60%) |
| Treatment | Well treatable with common antifungals | Difficult; combination therapy often required |
How Is Candida auris Transmitted?

Route of transmission: Direct or indirect contact via hands or surfaces (fomite transmission). The fungus survives for weeks on dry surfaces.
No airborne spread: There is no droplet transmission. Hygiene—especially hand disinfection—is key.
Colonization vs. infection: Many people are only carriers without symptoms. Disease occurs when the organism invades the body [4,5].
Who Is at Particular Risk?
- Severely ill hospitalized patients
- Immunocompromised individuals (e.g., on chemotherapy or with HIV)
- Patients with catheters or ventilator tubes
- Nursing-home residents with chronic illnesses
- Patients with frequent prior antibiotic/antifungal exposure
Symptoms
Superficial colonization: usually asymptomatic.
Local infections: e.g., ear, wound, or urinary tract infections.
Systemic infections (sepsis): high fever, chills, potential organ failure.
Diagnosis: Only laboratory testing confirms the organism. Susceptibility testing is essential to guide therapy [3,4,5,6].
Treatment
- Azoles: e.g., fluconazole—often ineffective.
- Echinocandins: first-line therapy, administered intravenously.
- Polyene antifungals: e.g., amphotericin B—reserve for resistance.
Asymptomatic colonization is not treated—hygiene takes priority. Close monitoring is required.
Prevention
- Strict hand hygiene
- Isolation of infected patients
- Protective clothing for staff
- Regular surface disinfection
- Screening of contacts
- Mandatory reporting where required
Current Spread
Worldwide: Cases on all continents; >40 countries affected.
Europe: >4,000 cases (2013–2023), notably in Spain, Greece, Italy, Romania, and Germany.
Germany: 2023: 77 cases; no known deaths, but increasing trend. [1,2,3,5,7]
Conclusion
Candida auris is a dangerous healthcare-associated fungus with extensive resistance. Usually harmless for healthy people, but potentially fatal for the immunocompromised.
Key: hygiene, vigilance, and prevention remain the most effective safeguards.
References
- ECDC (2025) – Drug-resistant fungus Candidozyma auris confirmed to spread rapidly in European hospitals
- ECDC (2025) – Survey on the epidemiological situation…
- Apotheken Umschau (2024) – Candida auris: How dangerous is infection?
- NetDoktor (2023) – Candida auris infection – a dangerous yeast
- CDC (2024) – Candida auris – Antifungal Resistance
- Egger et al. (2022) – The rise of Candida auris
- Du et al. (2020) – Candida auris: Epidemiology, biology, antifungal resistance