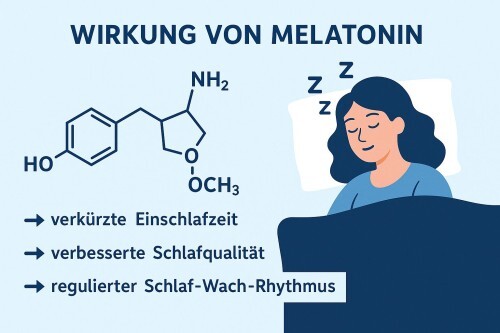
Sleep disorders are among the most common complaints in old age and during menopause. Symptoms range from early tiredness and frequent waking to severe difficulty falling asleep, hot flashes, and non-restorative sleep. A key role is played by the hormone melatonin, which regulates the sleep-wake cycle and whose production decreases significantly with age. But what does this mean in concrete terms? Can taking melatonin help you sleep better again?
Melatonin: Understanding the Sleep Hormone
Melatonin is the central hormone for the sleep-wake cycle. It is produced in the pineal gland and signals to the body that it is nighttime. As we age, the bodys natural production declines:
- The pineal gland calcifies over time, which restricts hormone production.
- Light signals reach the internal clock less effectively.
- The result is reduced nighttime secretion, leading to difficulty falling asleep or lighter sleep.
Older adults and women going through menopause are particularly affected, as hormonal changes make them more prone to sleep disturbances and more likely to report problems with falling or staying asleep.
Melatonin in Aging: Opportunities and Challenges
As we age, not only does melatonin production decline, but the overall sleep architecture changes as well—that is, the distribution and quality of different sleep phases. This explains why many older adults feel less refreshed in the morning, even if they sleep about as long as they did when they were younger.
A central factor is the decline in deep sleep (slow-wave sleep). Older adults spend less time in this particularly restorative sleep phase, which is important for recovery, the immune system, and memory. At the same time, more nighttime awakenings occur, fragmenting sleep. As a result, sleep may not be shorter, but it feels noticeably less restorative. Another phenomenon is the so-called “early bird” effect. With increasing age, the circadian rhythm shifts forward. Many older people become sleepy in the early evening and wake up very early in the morning.
Another aspect is the reduced adaptability of the internal clock. The bodys central timing system becomes less responsive to external cues like light or activity with age. This makes it harder to adjust to changes in sleep patterns. Seasonal differences in daylight (long summer days or dark winter months) also have a stronger impact than they did at a younger age.
Benefits of Melatonin in Aging
Melatonin can help older adults relieve sleep problems such as difficulty falling asleep or frequent nighttime awakenings. Studies have shown that especially prolonged-release melatonin is effective in treating insomnia in older adults and improves sleep quality.
- Falling asleep: Prolonged-release melatonin significantly shortens sleep latency.
- Sleep duration: Slight increase in total sleep time.
- Sleep quality: More stable nights with fewer interruptions.
- Proven in older adults: Helpful in primary insomnia with reduced endogenous melatonin production.
- Additional benefits: Less daytime fatigue and improved well-being.
However, melatonin is not a cure-all. Since age-related sleep problems usually have multiple causes, supplementation alone cannot solve all symptoms. The greatest benefit arises when melatonin is integrated into a multimodal approach combining sleep hygiene, targeted light management, and regular physical activity.
Melatonin and Sleep During Menopause
About 40–70% of women experience sleep problems during menopause. These issues are not just occasional—they can persist over long periods and significantly affect quality of life. A combination of physical and hormonal changes during this phase is responsible:
Hormonal Fluctuations (Decline in Estrogen and Progesterone)
During peri- and postmenopause, the levels of these hormones drop sharply. Estrogen normally promotes sleep by supporting the production of serotonin and melatonin. Progesterone has a calming effect on the nervous system. When progesterone levels fall, it becomes harder to fall asleep and maintain continuous sleep.
Hot Flashes and Night Sweats
A typical symptom of menopause is vasomotor instability. Hot flashes can cause sudden awakenings accompanied by intense sweating. These interruptions fragment sleep, allowing for less deep sleep and fewer restorative phases. Many women also report increased heart palpitations or inner restlessness during such episodes, making it even harder to fall back asleep.
Increased Risk of Sleep Apnea
After menopause, the risk of obstructive sleep apnea increases significantly. Causes include weight gain, hormonal changes, and decreased airway stability. In addition, the protective effects of estrogen and progesterone on the respiratory muscles and sleep architecture diminish. The condition often goes undiagnosed because many women are unaware that sleep apnea could be behind chronic fatigue, concentration problems, or morning headaches.

Melatonin in Menopause: Research Overview
Clinical studies with menopausal women have shown that melatonin shortens sleep latency, i.e., the time it takes to fall asleep. Participants also reported fewer nighttime awakenings and subjectively better sleep quality. These effects appeared mainly with use over a few weeks to months.
Other studies found no significant long-term effects. Long-term trials show that the effect may diminish after several months. One possible reason is that sleep disorders during menopause are multifactorial, meaning they are not caused solely by a melatonin deficiency.
Interestingly, melatonin also affects levels of oxidative stress and may indirectly improve sleep quality. It is not only a hormone but also a powerful antioxidant. It reduces free radicals, protects cells from oxidative damage, and supports mitochondrial function. During menopause, oxidative stress increases due to hormonal changes. Therefore, melatonin could have indirect anti-inflammatory and sleep-promoting effects, although evidence is not yet conclusive.
Natural Ways to Improve Sleep in Old Age
In addition to melatonin supplements, lifestyle plays a crucial role in achieving good sleep. Even small adjustments can stabilize the internal clock and improve sleep quality in the long term:
- Regular sleep schedule: Going to bed and waking up at consistent times trains the internal clock. Older adults especially benefit from this, as sleep tends to become lighter and more fragmented with age. A stable rhythm can reduce difficulties falling asleep.
- Light management: Light is the strongest regulator of melatonin production. Morning sunlight helps stabilize the day-night rhythm and synchronize the internal clock. In the evening, bright screens (phones, laptops, TVs) should be avoided or blue-light filters used, as blue light suppresses melatonin secretion.
- Exercise: Regular physical activity has been proven to improve sleep quality. Endurance sports such as running, cycling, or swimming are particularly effective. However, intense workouts should be avoided right before bedtime, as they can have a short-term stimulating effect.
- Relaxation techniques: Practices such as meditation, progressive muscle relaxation, or breathing exercises help reduce stress and racing thoughts. Even 10–15 minutes before bedtime can ease the transition into sleep.
- Optimal sleep environment: Darkness promotes natural melatonin production. Blackout curtains or a sleep mask can be helpful. Quiet surroundings and a cool room temperature of about 18–19°C are ideal, as the body slightly cools down for restorative sleep.
Safety and Side Effects of Melatonin
Before using melatonin to support sleep, its worth considering possible side effects and interactions. Although the sleep hormone is generally well tolerated, certain aspects should be kept in mind:
- Occasional mild side effects: gastrointestinal discomfort, morning drowsiness, headaches, and vivid dreams.
- No dependency or tolerance typically develops, unlike with conventional sleep medications.
- Caution is advised when taking melatonin together with blood pressure or diabetes medications, as interactions may occur.
Conclusion: Finding the Right Balance
Melatonin plays a key role in healthy sleep, especially in older age and during menopause when the bodys own production declines. While it is not a miracle cure, when combined with good sleep hygiene, light management, and healthy routines, it can be a valuable aid. The key is a holistic approach: Lifestyle measures form the foundation—melatonin is the supplement.
References
- Wade, A. G., et al. (2007). Efficacy of prolonged-release melatonin in insomnia patients aged 55–80 years: Quality of sleep and next-day alertness outcomes. Current Medical Research and Opinion.
- Li, J., Somers, V. K., & Lopez-Jimenez, F. (2018). Effects of melatonin on insomnia and other sleep disorders in postmenopausal women. Climacteric.
- Costello, R. B., et al. (2014). The effectiveness of melatonin for promoting healthy sleep: A rapid evidence assessment of the literature. Nutrition Journal.
- Hardeland, R. (2012). Melatonin in aging and disease — multiple consequences of reduced secretion, options and limits of treatment. Aging and Disease.
- Kalleinen, N., et al. (2012). Effects of melatonin on sleep and circadian rhythm in postmenopausal women. Menopause.