Electrolyte Loss & Hangovers: Understanding Alcohol Headaches
Hangovers result from complex biochemistry during alcohol metabolism. Two drivers stand out: fluid loss and electrolyte depletion (Na⁺, K⁺, Mg²⁺).
How alcohol dehydrates
Alcohol inhibits ADH, increasing urine output and dragging electrolytes with it. Even a few hours of drinking can lower sodium, potassium and magnesium.
Typical consequences
- Low sodium: brain dehydration → throbbing headache
- Low potassium: arrhythmias, weakness, fatigue
- Low magnesium: cramps, irritability, exhaustion
Alcohol metabolism strains the system
- Ethanol → acetaldehyde (toxic; nausea, palpitations, headache)
- Acetaldehyde → acetic acid → CO₂/H₂O or energy pathways
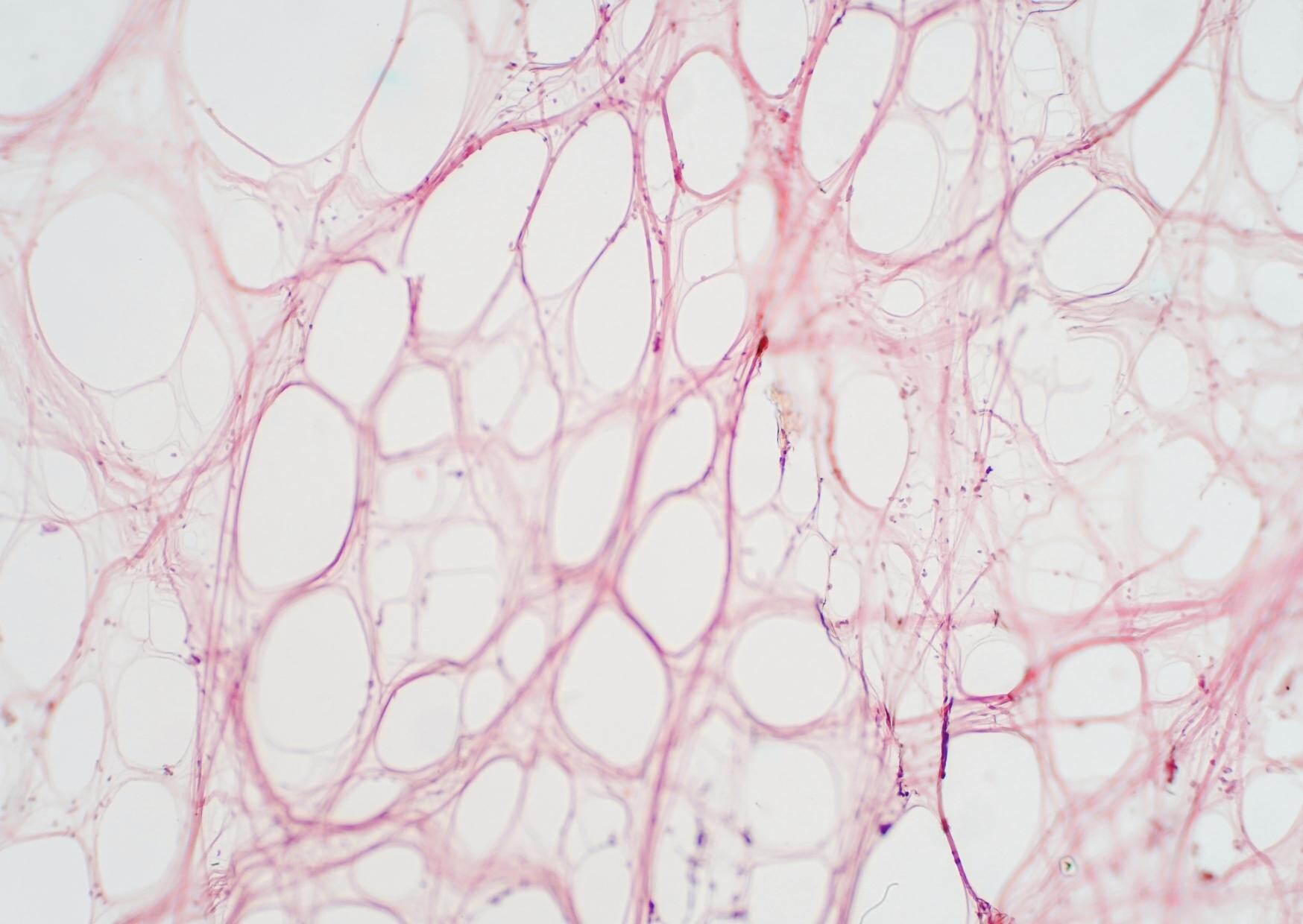
Processing requires water, shifts acid–base balance, raises energy demand and triggers oxidative/inflammatory responses. Slow ethanol clearance prolongs brain exposure and pushes oxidative stress into the second half of the night — worsening next-day symptoms.
Why headaches feel inevitable
- Dehydration slightly shrinks brain volume → meningeal pain
- Inflammatory mediators sensitise nociceptors
- Vascular constriction→dilation swings cause pulsation
- Glycaemic swings aggravate symptoms
Electrolytes: the key to recovery
Start prevention before drinking; hydrate and load electrolytes. During/after, use electrolyte solutions (preferably isotonic and sugar-free) with buffering capacity to stabilise acid–base and speed rehydration.
Bottom line
Hangovers reflect fluid/electrolyte loss, toxic intermediates and inflammation. Consistent rehydration with electrolytes is the single most effective step.
References: Wiese et al. (2000); Verster et al. (J Clin Med); Shirreffs & Maughan; Penning et al.
Passende Produkte zum Thema "Electrolyte loss & hangovers – alcohol headaches explained":
-
 €18.90
€18.90 -
 €19.90
€19.90